Overview glands (Glandulae):
exocrine glands:
endocrine glands:
Gl. = Glandula (Drüse); Gll. = Glandulae (Drüsen)
Glands (Terminologia histologica: Glandulae) usually
belong to the epithelia and are formed by
epithelial
cells specialised on production of secretions that are delivered into
the extracellular space which may be either the
lumen of an acinus or alveolus, the duct of an exocrine gland or may be
a capillary. However all cells that mainly
produce and set free substances are gland cells. This also involves fibroblasts
(connective tissue substanses and fibre components secreting cells), chondroblasts
(cartilage producing cells), osteoblasts (bone substance secreting cells),
plasma
cells or mast cells as typical connective
tissue cells, secreting
blood cells like
thrombocytes
as well as neurons that secrete
neurotransmitter substances.
There are many ways to classify glands regarding different points
od view:
A.) regarding whereto the secretion flows:
1. endocrine glands: The target of the secretion which is called
hormone in this case is the blood. After exocytosis
the hormone passes the basal lamina
of the gland cell, a minimal extracellular space filled with loose
connective tissue, the basal lamina
of an endothelial cell of a capillary
and finally an open pore of the endothelial
cell or a pore covered by a tiny diaphragm to reach the lumen of the
capillary.
The blood distributes the secreted hormone. In consequnce to this endocrine
glands are always rich in capillaries. Examples of endocrine glands are
the endocrine islands of Langerhans in
pancreas,
the pituitary, the pineal
gland, the adrenal gland, the thyroid
gland, the parathyroid gland, Leydig cells of the testis.
The enteroendocrine cells of the gut deliver their secretion to nearby
capillaries
or lymph vessels.
2. exocrine glands: The secretion is delivered either directly
into the lumen of an end piece (acinus, tubulus or
alveolus)
or a duct of an exocrine gland or into the lumen of the gut in case of
intestinal gland cells like goblet
cells. Examples of exocrine glands are the prostate,
the exocrine pancreas, the lacrimal glands,
sweat
glands, salivary glands, sebaceous
glands and the mammary gland.
B.) regarding the mechanism of secretion:
1.) merocrine
secretion, i.e. exocytosis, vesciles dock on and fuse with the
cell membrane and deliver their content
into the extracellular space without any notable loss of cell volume since
no cytoplasm gets lost. The secretion
product is water-like and non viscous in most cases. Eccrine secretion
is typical for: salivary glands, pancreas
and sweat glands
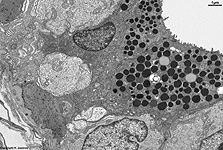
2.) apocrine secretion, i.e. apocytosis,
"secretory vesicles" that are lipid droplets
gather in the apical part of the cell close to the lumen, integral membrane
proteins of the cell membrane like Butyrophilin
bind to proteins associated to the border of the lipid
droplets thereby the latter begins to protrude into the lumen. By further
binding to the base of the spherical lipid droplets
the adjacent cell membrane fuses and
the lipid droplet, the surrounding small seam
of cytoplasm and the covering cell
membrane are released. Thus some cell
membrane and a little cytoplasm gets
lost with every secretion process resulting in a small reduction of the
cellular volume. The fat droplet is set free, when later on the surrounding
membrane collapses. This rare kind of secretion is only seen in the mammary
gland, apocrine sweat gland cells and the glands of Moll in the eyelid.
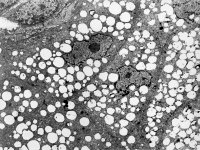
3.) holocrine
secretion, i.e. holocytosis, the whole gland cell fills up with
more and more "secretory vesicles" that in fact are lipid
droplets that may fuse. Thereby the epithelial
cell looses its contact to the basement
membrane and is pushed forward towards the lumen by proliferation of
the basal cell layer. The farer the cell gets to the basement
membrane the worse the situation for its nutrition by diffusion, thus
the cell begins to degenreate. The nucleus and
the cell organelles dissolve and the fatty,
sebaceous secretion product fills the whole cell. When contact to neighbouring
cells gets lost by desmosome disintegration,
the whole cell becomes the secretory product in that the cell
membrane finally disrupts and the rest of the cytoplasm
as well as the lipid droplets are released.
This type of secretion only occurs in sebaceous
glands and the glands of Meibohm or Zeiss of the eyelid.
4.) eccrine = avesicular secretion,
The majority of glands shows secretory vesicles, however, in case the chemical
properties of the secretion product (size, lipophily) do not require concentration
and packing in vesicles, secretory vesicles are not produced. A lot of
substances are secreted directly from the cytoplasm
of exo- or/and endocrine cells via more or less specific transmembrane
proteins. This is not visible in the electron microscope. The endocrine
pineal
gland is an example for an avesicular secreting gland. Its lipophilic
melatonin can easily pass the cell membrane
without need of any transporter. The liver
is an exocrine gland that secrets gall without any vesicles into bile
canaliculi and at the same time releases hundrets of other substances
via Disse's space into the blood, i.e. it is
exo- and endocine, in case one uses the expression endocrine not only for
hormones. Further examples of avesicular secretion is delivery of testosterone
by Ledig cells in the testis and the release of immunglobulins from plasma
cells to surrounding connective tissue.
Considering A and B, the following classification of glands results:
Gl. = Glandula (gland), Gll. = Glandulae (glands)
C.) considering morphology of the entire gland:
1a.) simple tubular singular glands e.g., glands of the stomach
or colon, sweat glands
1b.) branched tubular glands with several terminal pieces e.g.,
glands of the duodenum, cardia of the stomach,
Cowper's gland (Gl. bulbourethralis)
2a.) simple alveolar glands with a simple wide end piece e.g.,
small
sebaceous glands
2b.) branched alveolar glans e.g., larger sebaceous
glands, bronchial glands
3.) tubuloalveolar (wide end piece) or tubuloacinous
(narrow end piece) glands e.g., esophageal glands,
mammary gland,
prostate
4.) mixed tubular glands (many multiply branched end pieces
on a larger duct), z.B. lingual glands,
sublingual
gland (Gl. sublingualis)
5.) mixed tubuloalveolar -acinous glands e.g., tubuloalveolar:
lactating mamma; tubuloacinous: sublingual
gland (Gl. sublingualis), submandibular
gland (Gl. submandibularis), exocrine pancreas,
parotid
gland (Gl. parotidea)
6.) unicellular glands consisting only of one single cell e.g.,
goblet
cells
D.) considering morphology of the end pieces:
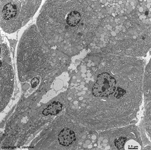
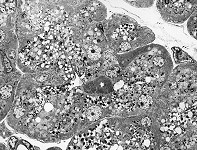
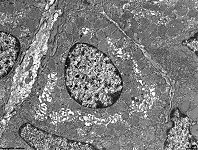
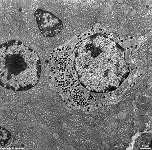
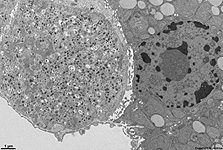
1.) serous end piece: acinus
(tiny lumen); round, mostly central nuclei;
secretory
vesicles concentrate in apical cytoplasm;
water-like secretion rich in proteins; eg., parotid
gland, exocrine pancreas
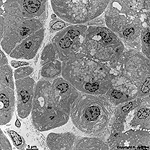
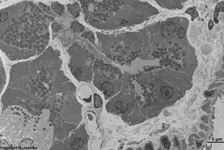
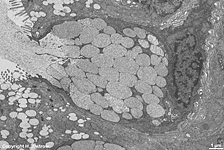
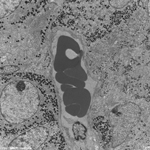
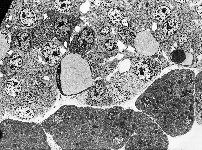
2.) mucous end piece: wider lumen in form of an alveolus
(nearly spherical lumen) or tubulus (tubular ending), the flat nuclei
seem to be pressed to the base of the cell, less electron-dense honeycomb-like
cytoplasm,
viscous secretion rich in acid mucins, e.g. goblet
cells
3.) von Ebner's half moon = a single layer of serous cells is
attached peripherically on a monolayer of mucous cells in an end piece;
only present in sublingual gland (Gl. sublingualis)
or submandibular gland (Gl. submandibularis).
E.) considering stimulation of secretion:
1.) glands with regulated secretion: secretion is evoked by chemical
or electrical stimuli, i.e. by hormones, neurotransmitters or electrical
depolarisation; e.g., pituitary, adrenal
gland, pancreas, stomach
2.) glands with constitutive secretion: permanent secretion without
defined stimuli; e.g. fibroblasts, hepatocytes,
plasma
cells
construction of a larger salivary gland:
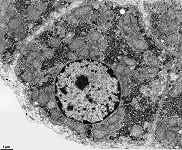
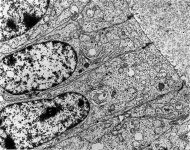
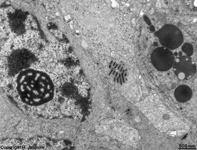
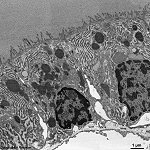
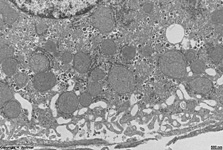
The major part of the secretion is produced by the epithelial
cells around the acini of the gland. Small intercalated ducts
with a monolayered cubic epithelium transport the secretion to an intralobular
duct whose monolayered columnar epithelial cells show a basal striping.
This striping is caused by regularly stacked mitochondria
in deep infoldings of the cell membrane
(--> example image) and is
visible in light- and electron microscopy. When the duct leaves the lobe
of the gland, it becomes an interlobular duct and is surrounded
by connective tissue. The columnar epithelium
begins to show an additional basal cell layer, i.e. is bilayered. In case
of larger glands such ducts join to form a main excretory duct which
has a pseudostratified epithelium.
--> secretory vesicles, salivary
glands, epithelium
--> Electron microscopic atlas Overview
--> Homepage of the workshop
Page & copyright H. Jastrow.